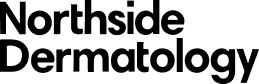
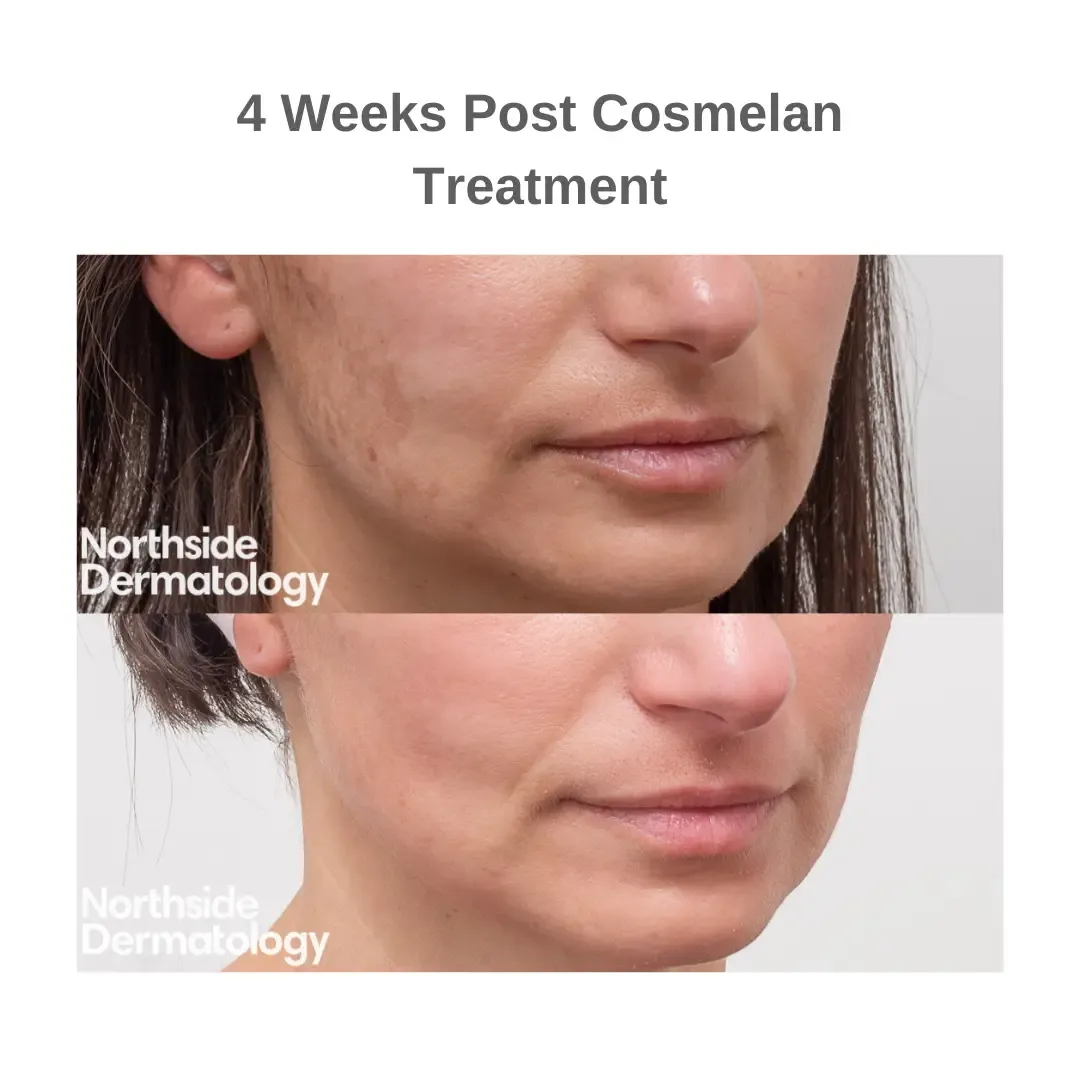
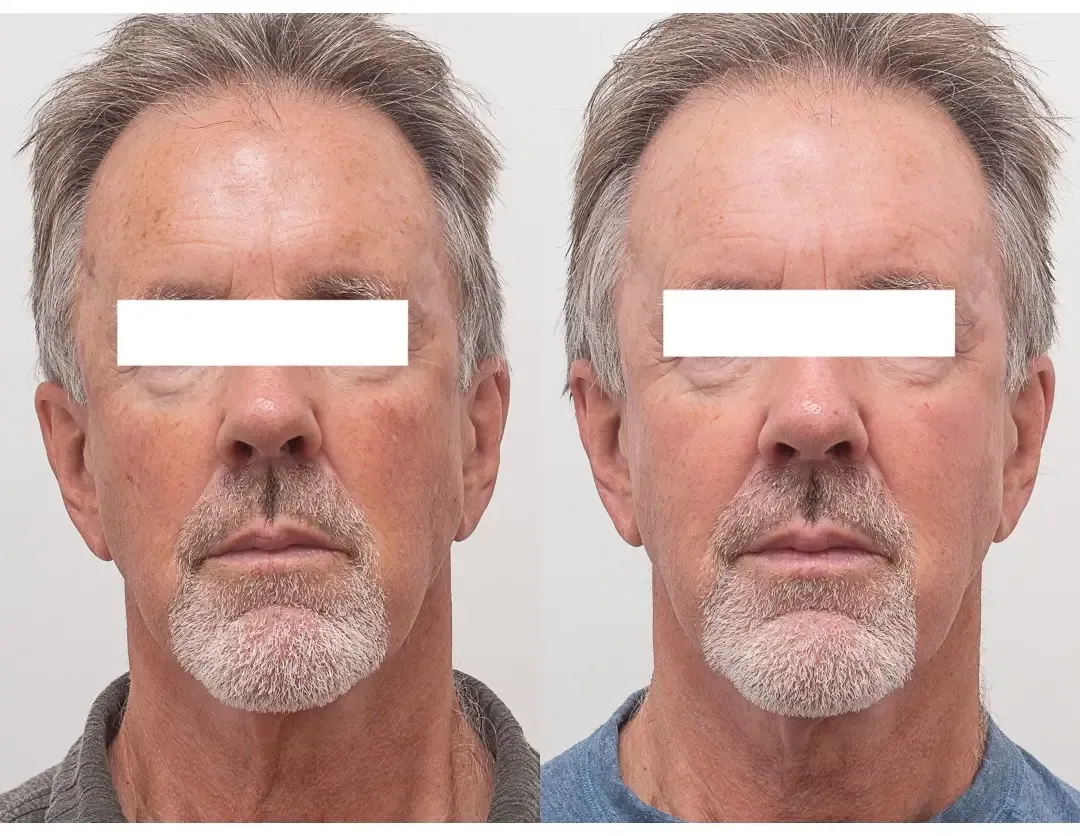
There are many causes of unwanted skin pigmentation. One of the most common pigmentation concerns is melasma, a condition where patients develop patchy areas of darker skin on the face and sometimes on nearby areas of the body. Melasma is best managed with a medical approach under the guidance of a specialist dermatologist.
Melasma usually appears as brown patches on areas that are regularly exposed to the sun. It most often arises on the face, particularly the forehead, cheeks, nose, upper lip and chin, but it can also affect the arms and back. Women are more likely to develop melasma than men, and people who tan easily or naturally have a darker skin tone are also more prone to it.
Although melasma does not affect physical health, it can be a source of embarrassment or anxiety about appearance. For those seeking treatment for melasma in Melbourne, specialist dermatologist-led care provides the safest and most effective results.
Melasma is categorised into three primary types
- Epidermal: Epidermal melasma is characterised by the presence of excess melanin in the outermost layers (epidermis) of the skin. The pigmentation is brown with well-defined borders. Epidermal melasma is typically more responsive to treatment.
- Dermal: Dermal melasma is identified by the presence of cells that ingest melanin, called melanophages, in the middle layer (dermis) of the skin. The pigmentation is brown, blue or grey with poorly defined borders. Dermal melasma is harder to treat.
- Mixed: Mixed melasma includes both the epidermal and the dermal type. The pigmentation is brown-grey in colour. Treating mixed melasma can be difficult but some improvement can be achieved.
A dermatologist may use a specialised light called a Wood’s lamp to determine the location of the pigment and the type of melasma.